
Introduction
Diabetes is one of the most common metabolic disorders that is associated with many life-threatening complications which diminish the quality of life of the patient. Diabetes is mainly of two types: type 1 diabetes (T1D) and type 2 diabetes (T2D). T2D is the most common type of diabetes worldwide marked by an increased blood glucose level, frequent urination, excessive thirst and weight loss. In T2D, impaired receptors do not respond to insulin, eventually leading to insulin resistance while in T1D, there is a deficiency of insulin produced in the pancreas . It is a juvenile onset disorder which is characterized by pancreatic dysfunction due to autoimmune reaction of the body where beta cells continuously get destroyed, eventually leading to insulin deficiency . The definite cause of T1D is still a mystery. However, certain studies demonstrate the mechanism by which A1 beta casein from cow milk can lead to T1D3,4 . Mounting evidence now shows the association of the ever-rising vaccination doses and the rise in T1D around the world.
One highly sensitive method of C-peptide determination has shown that beta cells can be detected even up to 40 years after the clinical onset of the disease. These findings help patients in advanced stage, for example, it helps patients whose β-cell function was thought to have long ceased in getting benefit from interventions to preserve β-cell function or to prevent complications . A lot of effort has been made to regenerate beta cells in vitro by providing growth factors and by reprogramming/trans-differentiation of terminally differentiated cell types. However, none of these approaches have proved to be successful in growing beta cells in vivo due to shortage of donors. The inefficient technique of β-cell generation and the difficulty of growing β-cell in adult humans sufficiently force a patient to adhere to medication/insulin for his whole life . Dietary modification and lifestyle change can play an important role in reversal of T1D and T2D by restoring the glucose levels to non-diabetic range, thereby either decreasing or eliminating the need of medicine/insulin.
Case presentation
Here, we present a case of a five-year-old boy, weighing 18 kgs, who was diagnosed with T1D in California, USA on 28.11.2022. Before diagnosis, he complained of frequent urination, increased thirst, excessive weakness and some weight loss. On the day of diagnosis, his Hb1Ac was 9.8% and blood glucose showed extreme fluctuations, with average postprandial glucose (PPG) above 300 mg/dl, the highest recorded was 490 mg/dl on 30.11.2022. It was an indication of T1D. The doctor concerned prescribed insulin injections to control blood glucose. He was advised to inject a total of 12 units of insulin daily. In the absence of initial C-peptide and Glutamic Acid Decarboxylase (GAD) reports, it was difficult to ascertain the diagnosis to be T1D. However, such negligence in maintaining records by the clinical practitioners should be avoided which may lead to discrepancies in diagnosis.
The parents approached the author on 8.12.2022 and agreed to put the patient on a plant-based wholefood diet immediately. The boy was put on a dietary modification plan and was supervised by the author through daily phone appointments. This diet was divided into breakfast, lunch and dinner. Breakfast included three different types of fruits which weighed 1% to 2% of body weight (in kilograms). In this case it was between 180 and 360 grams of fruits in breakfast. Lunch included three different types of raw vegetables which weighed 0.5% to 1% of body weight along with a customized vegan meal recipe. In this case it was 90 to 180 grams of raw vegetables followed by a customised vegan meal recipe. Dinner was calculated the same way as lunch. In addition to this, soaked nuts and sprouts were also a part of the diet programme and the quantity of these was equal to 0.1% of body weight. In this case it was about 18 grams each. Packed, processed and refined foods were strictly eliminated from his diet. Animal food, dairy products and oil were eliminated from the diet as these have shown to have a negative effect on diabetes. Blood glucose readings were regularly monitored and essential changes in the diet schedule were made as and when required. The parents were also in touch with the doctor concerned regularly for assistance in adjustment of insulin dosage.
Results
Before intervention: The patient had been suffering from T1D for two weeks as was diagnosed on 28.11.2022. His HbA1c was 9.8% and blood glucose was 490 mg/dl at the time of diagnosis. He was prescribed long-acting Lantus insulin 6 units in the morning and Humalog rapid insulin 2 units after breakfast, lunch and dinner. His fasting blood glucose level ranged from 110 mg/dl to 155 mg/dl with 12 units of total insulin per ay. His PPG ranged from 100 mg/dl to 300 mg/dl with 12 units total insulin per day. There were a few episodes of hypoglycemia with blood glucose levels dropping below 70 mg/dl.
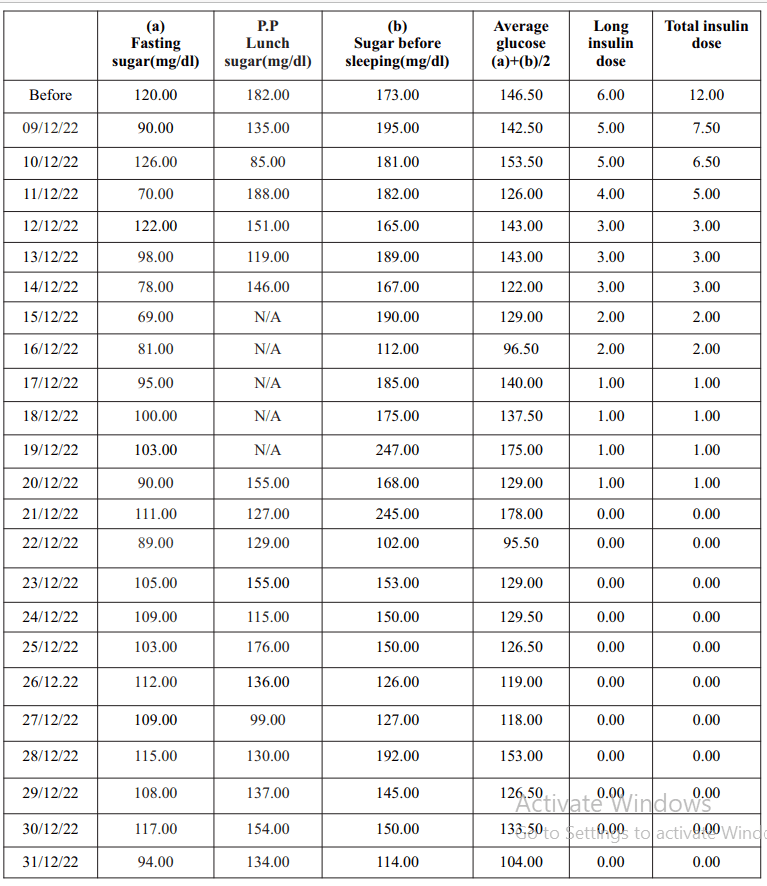
Post intervention: HbA1c was 7.3% post dietary intervention recorded on 10.01.2023. His average fasting b l o o d g l u c o s e l e v e l w a s 1 0 6 m g / d l (21.12.2022–31.12.2022). His average PPG was 136 mg/dl during the same period. The patient was able to eliminate his requirement of insulin injections on the thirteenth day (21.12.2022) of the dietary modification programme. He did not require insulin injections after 21.12.2022. He is no longer taking insulin injections. He is maintaining a normal glucose range by following the diet programme religiously. The patient was regularly monitored till 01.03.2023. His average fasting blood glucose level was 100 mg/dl and average PPG was 131 mg/dl during the month of February 2023.
Discussion
T1D has been neglected for a long time and its nationwide prevalence is not yet known. The growing number of T1D cases is a cause of concern as its treatment is difficult in comparison to that of T2D. In this article, we show a comprehensive analysis by stating the difference of blood glucose changes before and after the dietary intervention in a case of suspected T1D who approached us in December 2022. He was diagnosed with diabetes at the age of five and from the very first day he was on insulin. None of his parents have diabetes. His pre-intervention HbA1c reading was 9.8%, which is on the higher side. All the evidence so far defines him as a T1D case than any other type of diabetes. His higher values of HbA1c are suggestive of diabetic complications which was evident by his excessive urine, thirst, weakness and weight loss. His insulin dependency was eliminated within 14 days of switching to a whole food plant-based diet full of fresh fruits and raw vegetables. Presently, he is no longer dependent on insulin. His glucose levels are also in the non-diabetic range without insulin. He is adhering to regular follow ups.
Cases of T1D are increasing around the world. The possible cause can be genetics triggered by a wrong choice of food habits, including consumption of processed milk of A1 cows and increasing number of vaccine doses in the schedule4. Dietary modification is a great assistance to medical science in controlling diabetes to a large extent, without causing any side effects. The complete reversal of T1D through dietary modification is a ray of hope to many who are living a disheartened life administering insulin injections thrice a day to their children.
Conclusion
Diet and lifestyle play a major role in the reversal of autoimmune diseases like T1D9 . If left untreated, T1D can lead to severe complications. T1D was once thought to be irreversible and progressive after diagnosis, but emerging evidences suggest it can be reversed by following an appropriate diet plan. Here, we successfully treated a patient suffering from T1D by prescribing a customised diet plan. The patient was able to eliminate insulin dependency within 14 days of the dietary modification programme. This case study will serve as a ray of hope for the T1D patients and their distraught parents around the world.